- What Is The 340B Drug Pricing Program?
- The Role Of Contract Pharmacies
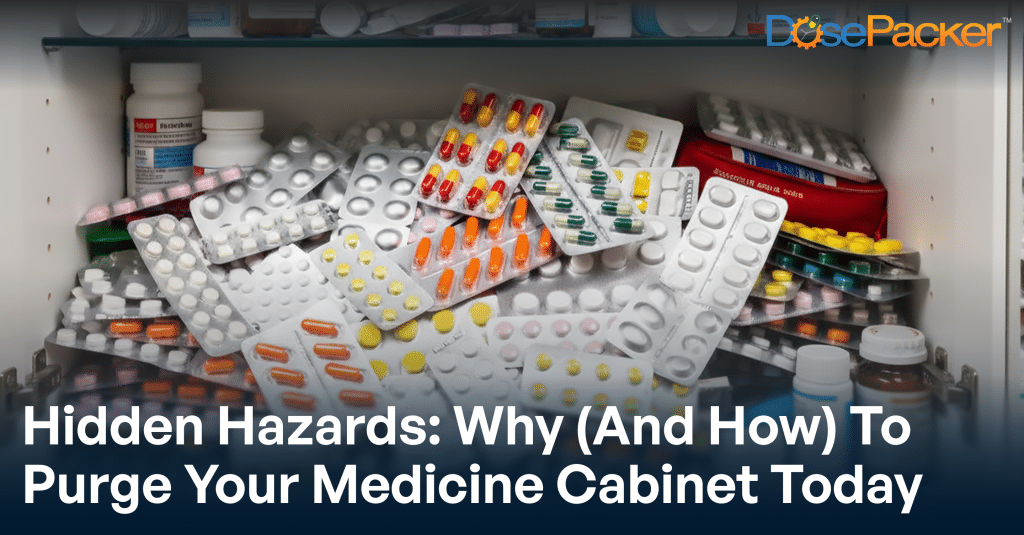
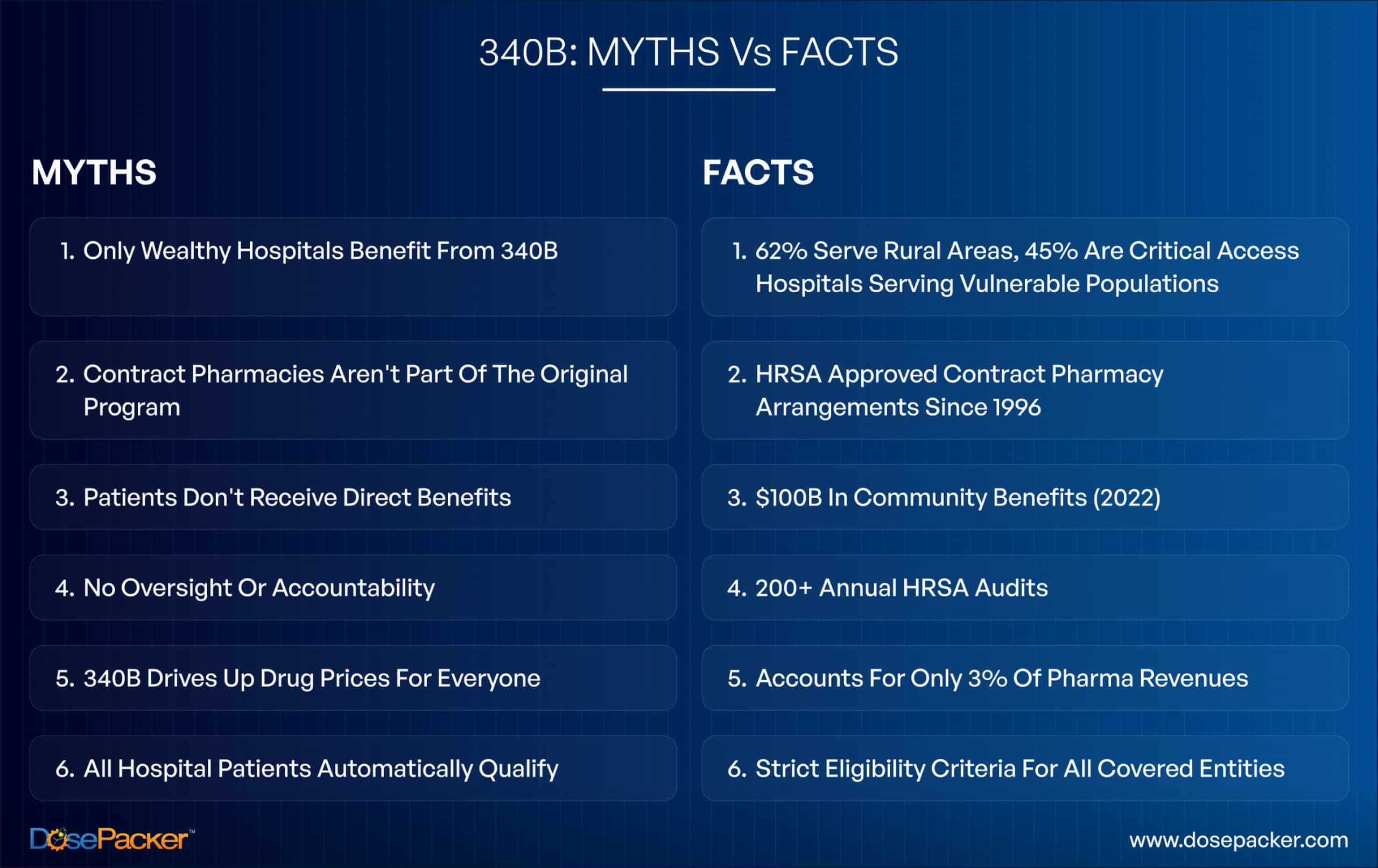
- Myth #1: 340B Only Benefits Large, Wealthy Hospitals
- Myth #2: Contract Pharmacies Aren't Part Of The Original Program
- Myth #3: Patients Don't Receive Benefits From The 340B Drug Pricing Program’s Savings
- Myth #4: There's No Oversight Or Accountability
- MYTH #5: 340B Drives Up Drug Prices for Everyone Else
- Myth #6: All Patients At 340B Hospitals Automatically Qualify
- Navigating Current Challenges With Confidence
- What This Means For Healthcare Providers: Opportunity Awaits
- The Bottom Line: A Program That Works
Unlock the latest in medication management technology and grow your care community with us.

Picture this: A small rural hospital administrator stares at medication costs for uninsured diabetes patients. The budget won’t stretch far enough. Then she discovers the 340B drug pricing program, a lifeline that could save her facility hundreds of thousands annually. But conflicting information online leaves her confused about whether it’s too good to be true.
She’s not alone. The 340B program reached $66.3 billion in discounted drug purchases in 2023, yet misconceptions about how it works persist among healthcare providers and the public. These myths can prevent organizations from maximizing benefits or cause unnecessary compliance anxiety.
Let’s separate fact from fiction.
What Is The 340B Drug Pricing Program?
Created in 1992 under the Veterans Health Care Act, the 340B drug pricing program requires pharmaceutical manufacturers to provide outpatient drugs at discounted prices, typically 20-50% off, to eligible healthcare organizations. These “covered entities” include safety-net hospitals, federally qualified health centers, and other providers serving vulnerable populations.
The genius of 340B? It’s not taxpayer-funded. Manufacturers participate to maintain access to Medicaid and Medicare markets. In exchange, they provide discounts that help safety-net providers stretch limited resources to reach more patients and expand services.
Named after Section 340B of the Public Health Service Act, the program operates on a simple principle: to enable covered entities to purchase drugs at reduced prices, allowing them to afford comprehensive care for communities that need it most.
The Role Of Contract Pharmacies
Not every covered entity operates an in-house pharmacy. That’s where contract pharmacies come in. These retail, independent, or specialty pharmacies dispense 340B medications on behalf of covered entities, essentially serving as an extension of the covered entities themselves.
As of 2026, over 32,000 pharmacy locations participate as contract pharmacies across the nation. The arrangement expanded significantly after 2010, when HRSA guidance clarified that covered entities could use multiple contract pharmacies to reach their patient populations.
For healthcare providers seeking to optimize their participation, specialized services like DosePacker’s 340B contract pharmacy solutions help ensure compliance while maximizing patient access, a critical consideration in today’s complex regulatory environment.
Myth #1: 340B Only Benefits Large, Wealthy Hospitals
The Fact: Walk into most 340B hospitals and you won’t find marble lobbies or luxury amenities. Instead, you’ll find that 62% are located in rural communities and 45% are specifically designated as critical access hospitals, facilities that serve as the only healthcare option for miles.
According to American Hospital Association data, many 340B participants operate on razor-thin margins. They use program savings to keep emergency rooms staffed, maintain 24/7 pharmacy access, and provide services that would otherwise be financially impossible.
The “wealthy hospital” narrative overlooks a fundamental truth: Wealthier hospitals don’t need the 340B program. The program exists precisely because certain providers serve disproportionate numbers of low-income, uninsured, and vulnerable patient populations that generate significant uncompensated care costs.
Myth #2: Contract Pharmacies Aren’t Part Of The Original Program
The Fact: Critics note that “contract pharmacy” is not mentioned in the 1992 statute. True. But here’s what the law actually requires: manufacturers must provide discounted drugs to covered entities, period. The statute doesn’t dictate how those drugs reach eligible patients.
HRSA has permitted contract pharmacy arrangements since 1996, just four years after the program’s creation. Congressional Research Service analysis confirms that the statutory language focuses on what happens (discounted drugs reaching eligible patients), not where it happens (in-house vs. contract pharmacy).
Think of it this way: If a hospital lacks an in-house pharmacy, should its patients be denied 340B benefits? Contract pharmacies address a logistical challenge while upholding program integrity through effective tracking and compliance measures.
Myth #3: Patients Don’t Receive Benefits From The 340B Drug Pricing Program’s Savings
The Fact: This might be the most damaging myth because it fundamentally misunderstands how 340B works. In 2022 alone, 340B hospitals provided nearly $100 billion in community benefits, a 47% increase from 2019, according to the AHA community benefit analysis.
Here’s how the savings flow works: A hospital purchases medications at the 340B discounted price. When dispensed to patients with insurance, the insurer pays at standard rates. The difference between what the hospital paid and what insurance reimburses generates revenue that gets reinvested in patient care.
Where does that money go? Free care for uninsured patients. Medication assistance programs that cover copays and deductibles. Behavioral health services. Mobile health units that reach underserved areas. Community health initiatives addressing food insecurity and housing instability.
A patient might not see a direct discount at the pharmacy counter. Still, they benefit when that same hospital offers sliding-scale fees, charity care, or disease management programs funded by 340B savings.
Myth #4: There’s No Oversight Or Accountability
The Fact: HRSA conducts approximately 200 annual audits of covered entities to ensure compliance with 340B rules. These aren’t rubber-stamp reviews. Auditors verify that 340B drugs are dispensed only to eligible patients, duplicate discounts aren’t occurring (i.e., 340B pricing cannot be combined with Medicaid drug rebates), entities maintain proper patient records, and contract pharmacy arrangements comply with regulations.
According to GAO reports on 340B program oversight, audit findings regularly lead to corrective action plans, repayments to manufacturers, and, in severe cases, removal from the program.
Beyond federal oversight, eight states enacted laws as of late 2024 requiring additional reporting and transparency from 340B entities. Hospitals must document how they use 340B savings and demonstrate community benefit.
The accountability framework protects both patients and the program’s integrity. Organizations that embrace compliance find themselves better positioned to maximize benefits while maintaining the documentation that demonstrates their community impact.
MYTH #5: 340B Drives Up Drug Prices for Everyone Else
The Fact: Let’s talk numbers. The 340B program accounts for only 3% of global pharmaceutical revenues. Drug companies provided an estimated $46.5 billion in 340B discounts in 2022, which is substantial but a fraction of the $347 billion in revenue growth by manufacturers between 2017 and 2022.
HRSA 2023 covered entity purchase data shows that while 340B purchases have grown, so have overall pharmaceutical profits. If 340B discounts drove price increases, we’d expect to see pharmaceutical profit margins shrinking. Instead, they’ve expanded.
Drug pricing is a complex process, driven by factors such as patent protections, market exclusivity, rebate negotiations with pharmacy benefit managers, and manufacturer pricing strategies. The evidence doesn’t support the claim that safety-net provider discounts significantly impact broader market pricing.
What the data does show: The 340B program effectively channels resources to organizations serving patients who need help most, without creating the adverse market effects critics suggest.
Myth #6: All Patients At 340B Hospitals Automatically Qualify
The Fact:Patient eligibility is strict and frequently misunderstood. To qualify for 340B pricing, patients must meet three specific criteria outlined in HRSA patient eligibility guidelines:
- An established relationship with the covered entity, documented in medical records.
- Healthcare services provided by the covered entity’s employed or contracted providers.
- Services consistent with the grant or designation through which the entity qualified for 340B.
Insurance status doesn’t determine eligibility. A privately insured patient seeing a covered entity’s oncologist for cancer treatment qualifies. An uninsured patient who walks into a 340B hospital’s emergency room for a broken arm might not qualify if they’re not receiving ongoing care consistent with the entity’s designation.
Understanding these requirements isn’t just about compliance; it’s about ensuring the program serves its intended beneficiaries while building sustainable systems that withstand scrutiny.
Navigating Current Challenges With Confidence
The 340B landscape has evolved since 2020, when some pharmaceutical manufacturers restricted access to contract pharmacies, citing concerns about program integrity. Multiple federal courts ruled that HRSA lacks statutory authority to penalize these restrictions. Eight states responded by passing laws protecting contract pharmacy access within their borders.
Here’s the encouraging reality: despite legal complexities, the program continues serving millions of patients effectively. Forward-thinking healthcare providers are adapting through stronger compliance frameworks, better documentation systems, and strategic partnerships.
Organizations that invest in proper 340B infrastructure find themselves well-positioned regardless of how regulatory debates resolve. The key is building systems that ensure program integrity while maximizing community benefit.
What This Means For Healthcare Providers: Opportunity Awaits
Understanding 340B opens doors to expanded services and enhanced community impact. The organizations seeing the most significant success share common approaches:
- They prioritize patient eligibility verification through systems that document provider-patient relationships and ensure services align with their 340B designation.
- They implement proactive compliance measures that prevent duplicate discounts and maintain audit-ready documentation.
- They partner strategically with experienced providers who understand regulatory nuances and can help navigate evolving requirements.
Working with specialized partners who understand these complexities, from eligibility verification to regulatory compliance, accelerates success while reducing risk. The right systems and processes protect your organization while unlocking resources that transform community health outcomes.
The Bottom Line: A Program That Works
The 340B program represents one of the most effective public-health partnerships in American healthcare. When implemented thoughtfully, it enables safety-net providers to extend their reach, expand their services, and improve outcomes for vulnerable populations.
Consider the rural hospital administrator we mentioned earlier. After implementing a well-structured 340B contract pharmacy partnership, her facility saved $380,000 in the first year. Those savings funded a diabetes management program that resulted in a 23% reduction in hospitalizations among participating patients. Two years later, they introduced a medication assistance program that has helped 450 low-income patients maintain treatment adherence.
That’s not a myth or a theoretical benefit; it’s a proven fact. That’s 340B working exactly as Congress intended, channeling pharmaceutical discounts to organizations that transform them into better health for communities that need it most.
The path forward is clear: understand the facts, implement robust compliance systems, partner strategically, and focus on what matters most – the patients and communities you serve. The 340B program gives you the tools. Your mission gives you the purpose. Together, they create opportunities to make a meaningful difference.